Hepatobiliary system disorders in cats
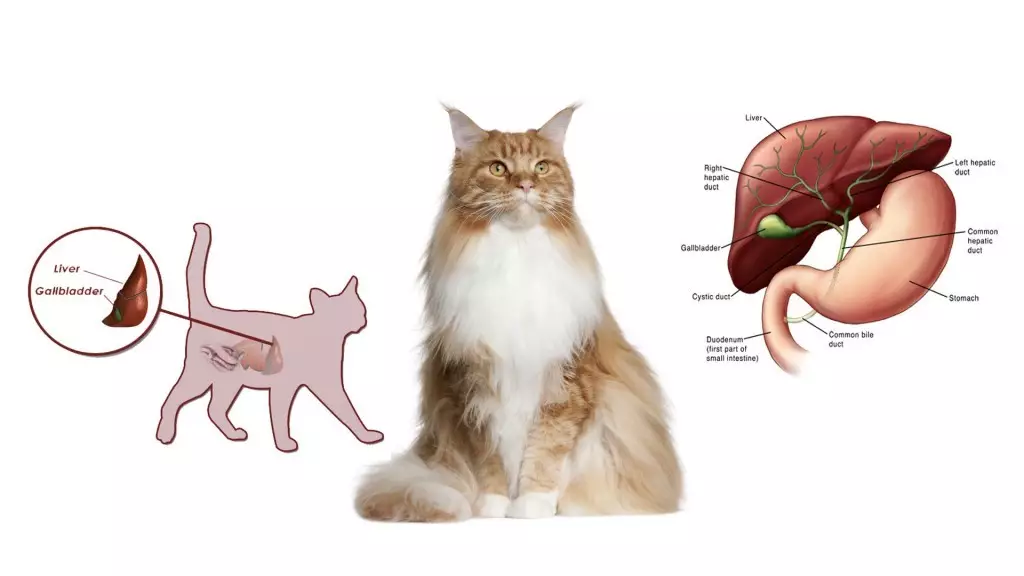
What is the hepatobiliary system?
The term “hepatobiliary” means having to do with the liver, the gallbladder, bile ducts and bile. “Hepato-” refers to the liver and “-biliary” refers to the gallbladder, bile ducts or bile. One of the functions of the liver is to produce and secrete bile. The gallbladder, a pear-shaped organ that sits directly below the liver, stores excess bile, which is released via the bile ducts into the intestine when food is eaten, to help break down the fats and carry waste away.
The liver performs many complex functions in addition to its vital role of manufacturing the bile acids needed for digestion. Some of these are:
- Metabolising lipids (fats), carbohydrate, and protein
- Metabolising drugs (deactivating them or making it easier for the body to excrete them)
- Storing and metabolising vitamins
- Storing minerals, glycogen and triglycerides (fats)
- Manufacturing proteins needed for various body functions, such as blood clotting
- Detoxifying harmful substances produced by the body (such as ammonia) or consumed by the animal (such as poisons).
The liver has a large storage capacity and can regenerate; therefore, illness or injury must be considerable, chronic or recurrent to cause overt permanent damage or failure. However, as it is exposed to toxic compounds, it is susceptible to injury. When the liver does fail, the body has no way to compensate for the loss of this vital organ, and serious problems can result.
The most common liver disorders that occur in cats are hepatic lipidosis and feline cholangiohepatitis. For other conditions relating more specifically to the biliary system, see biliary tract disorder in cats.
Hepatic lipidosis (“fatty liver”)
Hepatic lipidosis, the most common liver disease in cats, occurs when an excessive amount of fat infiltrates into the liver. The disease is associated with a period of poor appetite (going without food for a few days to several weeks), especially in obese cats. As the fat accumulates in the liver, it becomes swollen and yellow. Yellow pigment is also released into the bloodstream, causing the whites of the eyes to turn yellow, a classic sign of a fatty and low functioning liver. Untreated, this condition can lead to liver failure and eventually death.

Feline cholangitis / cholangiohepatitis syndrome (CCHS)
Inflammatory liver disease is the second most common of the feline liver diseases. There are many causes of liver inflammation (also called “hepatitis”) in cats. Cholangitis refers to inflammation anywhere in the biliary tract. Cholangiohepatitis (also called “hepatobiliary disease”) refers to inflammation of the biliary tract and surrounding liver tissue (the difference between these two conditions depends on the location of the inflammation within the liver).
The inflammation and swelling resulting from cholangiohepatitis hinders the proper flow of bile, causing it to be retained in the liver and biliary ducts, creating a condition known as “stagnant liver.” Since bile is a highly acidic digestive fluid, if it is not flowing it can cause irritation, congestion, and significant tissue damage. This is a serious condition that requires immediate medical attention.
Cats with cholangiohepatitis typically suffer from other inflammatory conditions as well, including inflammatory bowel disease (IBD) and pancreatitis (inflammation of the pancreas). The concurrent inflammation of the three interrelated organ systems, the pancreas, liver and small intestines, is termed “feline triaditis”. These three conditions tend to occur together because the pancreatic duct that transports digestive enzymes to the intestine opens into the same port as the common bile duct. These two ducts share a common entryway to the intestine, therefore, if an overgrowth of bacteria from the gut, as a result of IBD, invades the entryway, both the liver and pancreas can also become inflamed and infected.
Feline cholangitis / cholangiohepatitis syndrome is the most common acquired inflammatory liver disease in domestic cats, occurring much more frequently than liver disease in dogs. It is prevalent particularly in the Himalayan, Persian and Siamese breeds. There are three subtypes:
- Neutrophilic (or suppurative, exudative or acute) cholangitis / cholangiohepatitis
usually causes obvious and sudden illness in cats and is typically seen in young or middle-aged adults. This type is associated with bacterial infection arising from the small intestine. - Lymphocytic (or nonsuppurative or chronic) cholangitis / cholangiohepatitis
usually affects middle-aged or older cats, who are often ill for months to years before diagnosis. This type is associated with white blood cells called lymphocytes that infiltrate the liver. - Biliary cirrhosis
is the rarest type, caused by scarring of the bile duct walls and the surrounding liver tissue and regarded as an end stage of chronic biliary tract disease.
Symptoms of hepatobiliary system disorders in cats
Cats with liver disease often look and feel very unwell. However, signs that a cat has liver disease can vary greatly. Common symptoms may include:
- Loss of appetite or fluctuations in appetite
- Vomiting
- Diarrhoea
- Dehydration
- Fever
- Lethargy
- Weakness
- Jaundice (a yellow tinged color to the gums or skin, best seen on the ears and eyes)
- Hiding in unusual places (e.g., closet)
- A swollen and painful abdomen
- Stomach ulcers
- Excessive urination
- Excessive thirst
- Enlarged liver
- Weight loss
- Gastrointestinal bleeding (occasionally)
- Blood clotting problems
Symptoms of hepatic lipidosis vary and can be very subtle, but can include in addition to the above:
- Complete loss of appetite for a prolonged period (anorexia)
- Rapid weight loss (more than 25% of body weight)
- Constipation or much reduced volume of faeces
- Excessive drooling (often a sign of nausea)
- Inability to hold up the head because of a weakened neck (the head hangs down more than usual with a chin tuck)
- Muscle loss and decreased body condition with retention of abdominal fat
If left untreated, or in severe cases, signs of liver failure can include the following:
- Black tarry stool
- Bruising (abnormal clotting)
- Coma (from the liver poisons building up in the body)
- Seizures
- Collapse
- Death
Causes of hepatobiliary system disorders in cats
Hepatic lipidosis, or fatty liver, is the most common feline liver disease, primarily affecting middle-aged cats. What causes the excessive accumulation of fat (triglycerides) within the liver? In many cases, this remains unknown, but the disease is often associated with an underlying primary disease that causes anorexia (a period of poor appetite for a prolonged period), setting the stage for hepatic lipidosis, especially in obese cats. In some situations, environmental stresses appear to be the cause of the cat’s inappetence.
Factors that are associated with anorexia include:
- A disease such as diabetes mellitus, pancreatitis or kidney disease that causes loss of appetite.
- A sudden change of diet (for weight loss or introducing a new food that is unacceptable to the cat).
- A stressful event (such as moving, boarding, introduction of a new pet, a new person in the home, getting lost, being locked up or death of other pets or owners).
Cholangiohepatitis is an inflammatory disorder which may in part be associated with an immune response to bacteria and/or dietary antigens (foods that induce an immune response in the body).
Conditions associated with the cholangitis/cholangiohepatitis syndrome include:
- Other inflammatory disorders, in particular, inflammatory bowel disease, pancreatitis, and kidney disease (chronic interstitial nephritis)
- Bacterial infections
- Blood poisoning (septicaemia)
- Gallstones
- Inflammation of the gallbladder
- Liver flukes
- Tumours
- Malformations or obstructions of the bile ducts
- Blockage of the gall bladder
- Gall bladder sludging

How are hepatobiliary system disorders in cats diagnosed?
In order to diagnose a hepatobiliary system disorder, the vet will begin with a detailed case history and physical examination. Blood testing can help detect and diagnose liver disease. X-rays and ultrasonography can help determine liver size and identify irregularities, gallstones, and diseases of the gallbladder.
Since the symptoms of various feline hepatobiliary disorders are similar, several diagnostic tests may be required to confirm the diagnosis and rule out other conditions. A definitive diagnosis usually requires biopsies to be taken from several parts of the liver. Tissue samples may be aspirated or biopsied for bacterial culture, cell and tissue analysis, and, if necessary, toxicologic analysis.
Diagnosis of hepatic lipidosis may be based on:
- Case history
- Physical examination findings
- Symptoms consistent with hepatic lipidosis
- Blood work, to evaluate the white and red blood cells, kidney and liver function, protein and electrolytes
- Abdominal ultrasonography, to examine the liver and gallbladder
- Aspirate or biopsy of the liver, guided by ultrasound
- Larger biopsy of the liver, performed surgically
- Analysis of aspirated or biopsied cells
Diagnosis of cholangiohepatitis may be based on:
- Case history
- Physical examination findings
- Clinical signs
- A complete blood count (CBC)
- Blood chemistry profile
- Urinalysis
- Bile acid analysis
- A blood-clotting test
- Abdominal X-rays and/or ultrasound
- An ultrasound-guided biopsy of liver tissue, to confirm the diagnosis and determine what form of cholangiohepatitis is present
- A needle aspiration of the bile and subsequent analysis by a pathologist
- Exploratory surgery if there is a bile duct obstruction
Prognosis
The prognosis for a hepatobiliary system disorder is highly variable and depends on the underlying cause of the disease. Additionally, the prognosis is much less optimistic where diagnosis is delayed until the disease is advanced.
In cases of hepatic lipidosis, the outlook is good if the diagnosis is made early, treatment is started promptly, and any underlying disease can be treated. Cats with concurrent pancreatitis tend to do more poorly. Recurrence of hepatic lipidosis is rare in cats who recover.
In cases of cholangiohepatitis, the outlook can be unpredictable. Many cats with the suppurative form of the disease who are diagnosed early and properly treated can make a full recovery. For cats with the non-suppurative form of the disease who are diagnosed early and treated promptly, long-term remission is possible. In cases where there is impeded bile flow, this will lead to complete liver failure and death unless the cause is found and corrected quickly.

Treatment for hepatobiliary system disorders in cats
Early treatment is vital for cats with hepatobiliary system disorders. The specific treatment prescribed will depend on whether an underlying cause can be identified. Where this is not possible, or where there is chronic or end-stage liver disease, treatment is geared towards slowing progression of disease, minimising complications, and allowing time for the liver to regenerate.
Supportive treatment may entail fluid therapy, medications to protect the liver, and nutritional support. Extremely ill cats may also receive intravenous fluids, electrolyte replacement, and vitamin supplementation in the initial stages of treatment. These supportive measures help to prevent other possible complications of hepatobiliary disease.
Nutritional support:
Dietary support is an essential element of treatment, including the provision of a good quality, highly digestible, high caloric diet. Prescription diets are available for cats with hepatobiliary disease, and the veterinarian will prescribe the appropriate formula to feed your cat during and after treatment.
Some liver disorders require modifications of fat or protein or supplementation with certain vitamins. It may be advised to feed small, frequent meals. Dehydrated or malnourished cats may require intravenous (IV) fluids for a period of time. Cats that refuse to eat may require temporary tube feeding.
Vitamin deficiencies can occur with liver disease. Prescribed vitamin and mineral supplements may include zinc, B vitamins, vitamin K, and vitamin E. Foods rich in vitamin K may be recommended to address blood-clotting issues, and zinc-rich foods to help prevent cirrhosis (scarring of the liver). It is important to always follow the veterinarian’s recommendations on dietary modification and vitamin supplementation because overdoses of certain vitamins can be harmful.
Treatment for hepatic lipidosis:
Untreated, hepatic lipidosis can result in liver failure and death; therefore, aggressive treatment is essential. A prescribed appetite stimulant may help if started early in the disease process; however, most of the time appetite stimulants are not effective and the use of a feeding tube is necessary. The veterinarian will recommend an appropriate food. Initially, feedings are small and given frequently.
Treatment for hepatic lipidosis typically requires round-the-clock care for several days and may also include the following:
- IV fluids to help treat dehydration
- Placement of a temporary feeding tube to provide adequate calories (this may be necessary for several weeks)
- A high-protein, calorie-dense, balanced diet
- Anti-vomiting medication
- Appetite stimulants
- Nutritional supplementation
- Antibiotics
- Vitamin K (to help fix clotting problems if abnormal)
- Plasma transfusions (if severe clotting problems are noted)
Treatment for cholangiohepatitis:
Because the causes of cholangiohepatitis are variable, the appropriate course of therapy is determined on a case-by-case basis, based on the identified cause. Treatment can take three to four months, and regular monitoring of liver enzymes will be required. Animals with non-suppurative cholangiohepatitis typically require long-term therapy, sometimes for the rest of their lives.
Depending on the identified cause, treatment may entail:
- Supportive fluid treatment to correct dehydration
- Surgery, where there is a physical obstruction in the bile duct or gall bladder
- Drugs to manage any infection or inflammation
- Antibiotics specifically targeted to the specific bacteria that are identified with culture and sensitivity tests will be given for 2 to 3 months in cases of neutrophilic (suppurative) liver disease (bacteria may produce toxins that are normally eliminated by the healthy liver but may accumulate in the afflicted cat)
- Choleretics, or drugs that thin the bile and improve biliary flow
- Antioxidants and other supportive supplements, which may decrease cell damage caused by biliary dysfunction and help the liver rebuild healthy functional tissue
- Applicable treatment where there is a concurrent condition such as IBD, pancreatitis or small intestine absorption issues
- Corticosteroids in cases of nonsuppurative (chronic) cholangiohepatitis because of the suspected immune-mediated aspect of this disease
In summary
The liver performs numerous functions, one of the most important of which is to help digest food by manufacturing and secreting bile. Disorders of the hepatobiliary system are conditions pertaining to or emanating from the liver, bile ducts and gallbladder. There are two commonly occurring hepatobiliary system disorders in cats which together comprise about two-thirds of feline liver diseases: cholangiohepatitis (inflammation of the liver and biliary tract) and hepatic lipidosis (fatty liver disease).
Cats with a hepatobiliary system disorder typically look and feel very ill. Symptoms may include vomiting, diarrhoea, loss of appetite, fever and jaundice. Obtaining a diagnosis of the particular type of hepatobiliary system disorder usually entails bloodwork, ultrasonography and liver tissue biopsy or aspiration. If there is an underlying disease that is causing or contributing to the condition, it is important that this is also diagnosed and treated appropriately. Treatment entails aggressive supportive therapy, which may include fluid treatment, dietary modification, vitamin supplementation, antibiotics and other appropriate drugs. The prognosis for cats with a hepatobiliary system disorder varies greatly, depending on the type of disorder, the promptness of diagnosis and treatment and the overall health of the animal.
Bow Wow Meow Pet Insurance can help protect you and your cat should an unexpected trip to the vet occur.
-
Find out more about our cat insurance options
-
Get an online pet insurance quote


More information
- https://www.merckvetmanual.com/cat-owners/digestive-disorders-of-cats/disorders-of-the-liver-and-gallbladder-in-cats
- https://www.msdvetmanual.com/digestive-system/hepatic-disease-in-small-animals/overview-of-hepatic-disease-in-small-animals
- https://www.petmd.com/cat/conditions/endocrine/c_ct_hepatic_failure_acute
- https://www.pethealthnetwork.com/cat-health/cat-diseases-conditions-a-z/fatty-liver-disease-cats-not-eating-can-quickly-kill
- https://healthypets.mercola.com/sites/healthypets/archive/2017/10/24/feline-cholangiohepatitis.aspx
- https://www.petmd.com/cat/conditions/digestive/c_ct_hepatic_lipidosis
- https://www.msdvetmanual.com/digestive-system/hepatic-disease-in-small-animals/feline-hepatic-lipidosis
- http://websource.4act.com/chaparralvet/?p=326







